A decade of compassionate, community care
Now in its tenth year, the Richmond Health and Wellness Program brings care coordination to the doorstep of vulnerable communities in central Virginia.
January 25, 2023 Kathie Falls, MSN, director of clinical operations of the Richmond Health and Wellness Program, takes the blood pressure of program participant James Peace. (VCU School of Nursing)
Kathie Falls, MSN, director of clinical operations of the Richmond Health and Wellness Program, takes the blood pressure of program participant James Peace. (VCU School of Nursing)
By Caitlin Hanbury and Sara McCloskey
University-sponsored health clinics are common across the country. But over the past decade, the Richmond Health and Wellness Program (RHWP), spearheaded by the Virginia Commonwealth University School of Nursing, has earned a national reputation as a model for holistic care coordination.
The program delivers weekly wellness clinics that focus on health assessment, monitoring, and coaching in five community-based sites across the Richmond region. Some of the things patients learn include effective chronic disease self-management and diet management through healthy cooking demonstrations as well as wellness coaching. The care helps them proactively manage other health issues and social needs before they develop into emergencies.
What makes this program unique are the connections participants build with students. About 100 VCU undergraduate and graduate learners essentially run the program with guidance of faculty members. In ten years, it has evolved by incorporating students from across a wide variety of VCU's health science disciplines who learn how to advocate and empower their participants to access the services they need.
An interprofessional educational model
Participants can take advantage of the clinic’s services either with a scheduled 30-minute wellness visit or as a walk-in for unplanned or immediate needs. Last year, 437 people utilized the program accounting for a total of 2,883 visits.
RHWP faculty members recognize how some Central Virginians have limited access to transportation, technology, or are not experienced navigating the complicated healthcare system. Kathie Falls, MSN, director of clinical operations for RHWP, says the program tries to identify gaps in care for participants and connects them to key services to help them manage their healthcare needs on their own.
Visits frequently center around helping residents understand their conditions and how to proactively manage them. Then, they’re connected to information and resources.
“By meeting people where they are and really listening to what’s important to them, we can tailor our services to their specific needs, which makes all the difference,” Falls said. “We’re here to advocate for people and empower them to ask for what they need. When necessary, we can step in and help them articulate their needs to providers and health care workers whether in the emergency room or in their primary care provider’s office. We can help them tell their story.”
Real life lessons of compassion
RHWP participants receive services from medical students, who are taught that compassion is at the core of providing care.
Kimberly Battle, Ph.D., clinical assistant professor in the Department of Family and Community Health Nursing, said the learning environment students experience in RHWP clinics plays an integral role in their understanding of the realities their participants face.
“We have to realize with our students that everyone comes from different backgrounds. It’s important to teach students compassion, to teach them how to relate so that they can integrate into their own practice, how they think about affordability. Having [the student] ask ‘Is this realistic? This plan that I am developing for my participant that I’m interacting with?’” she said.
Many students who start with RHWP to satisfy graduation requirements opt to continue their service. As a result, the VCU School of Nursing is working to create more opportunities so students can continue providing community service as they move toward graduation and look for jobs.
The continued dedication of students and faculty fosters a strong rapport with RHWP participants, which shows the quality of interactions these individuals have with members of the VCU campus community. Falls, in particular, has seen intergenerational connections grow between participants and students.
“Social isolation is a huge issue for older adults in general, particularly older adults with limited income. The pandemic absolutely made this situation worse,” Falls said. “Our participants open up to students about things they’ve been afraid to ask in the past. Maybe they’re embarrassed or haven’t been able to find the words, but they ask the students and they get an answer.”
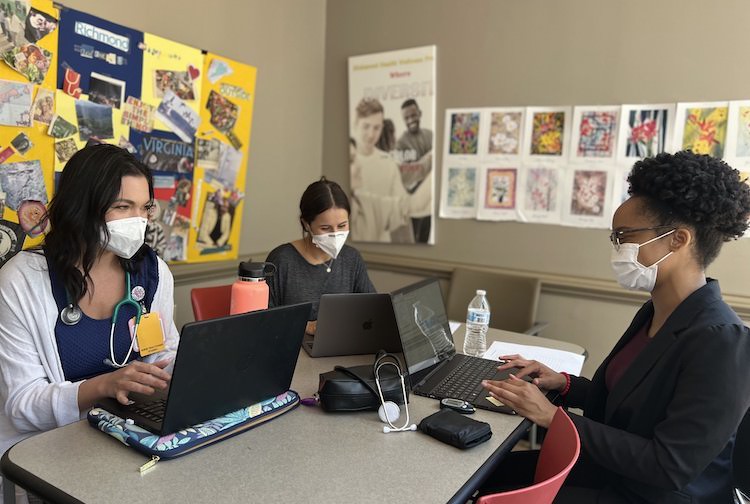
VCU health sciences students, like Kailey McCullen, Alexandra Bongiorno and Kam Davis (left to right), are the heart of the Richmond Health and Wellness Program. VCU faculty highlight how many students continue to be involved with the program even after fulfilling their degree requirements. (VCU School of Nursing)
New horizons for community-based care
With a decade of success as its foundation, RHWP continues to grow. A recent grant of nearly $4 million in funding from the Health Resources & Services Administration, an agency within the U.S. Department of Health and Human Services, will enable the program to reach new communities with the addition of a mobile van.
“We are taking our program on the road [...W]e have such a history with our program that we recognize that there are hot spots for chronic disease. We look forward to bringing the nursing students to these areas where we can bring our education and care coordination and start to build trust and rapport in these areas and establish these relationships,” Battle said.
The Mobile Health and Wellness expansion will include four sites: a library at the Southside Virginia Community College, a church in the Tappahannock-area, Gilfield Baptist Church in Petersburg and the Southwood Apartments community center in Richmond. The care coordination van is expected to be delivered by 2026, and will offer clinical services once a week in two of these designated locations.
In preparation to serve these communities, RHWP has worked closely with partner agencies in these areas over the past few months to build stronger relationships with community members as the program enters this new chapter of service.