Experts discuss barriers preventing patients from participating in clinical trials
Health equity panel discussion recommends researchers and doctors address long standing historical wrongs when talking to patients about joining clinical trials.
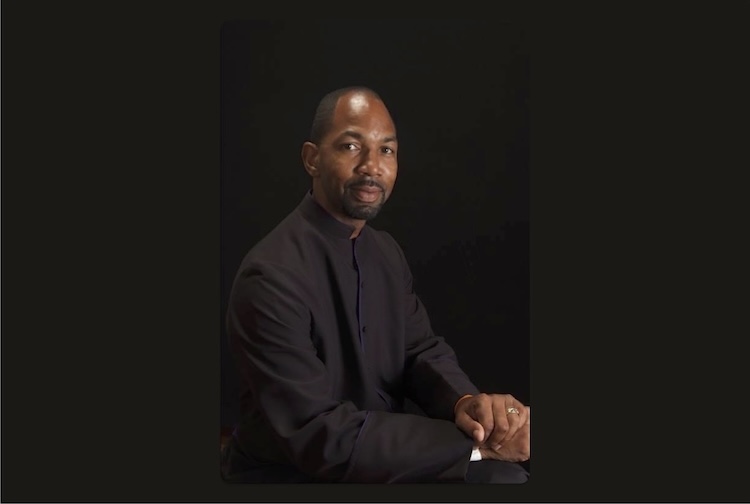
April 07, 2023 Experts and community advocates discussed how marginalized people in the U.S. are impacted by the history and procedures of clinical trials. (Getty Images)
Experts and community advocates discussed how marginalized people in the U.S. are impacted by the history and procedures of clinical trials. (Getty Images)
By James Shea and Sara McCloskey
The often inhumane treatment of Black and Brown people in the United States, some of whom were enslaved, during experiments and clinical trials continues to have a long-lasting effect on research conducted today.
Efforts to create more inclusive clinical trials were addressed in a recent panel discussion entitled “Skepticism Around Clinical Trials,” put on as part of the Virginia Commonwealth University Office of Health Equity's History and Health; Equitable Access to Care series. This programming, co-sponsored by the VCU Humanities Research Center, aims to educate the public, as well as Virginia Commonwealth University and VCU Health community members about disparities in healthcare access and creating better health outcomes.
Leslie Randall, M.D., MAS, director of gynecologic oncology at the VCU Massey Cancer Center, says scientific research must confront historic injustices because many people of color are reluctant to get involved in clinical trials because of several major incidents. These include the federally funded Tuskegee Institute study, where Black men with syphilis were studied without informed consent and went untreated even though medicine became more widely available, and the identification of the HeLa cell line through research conducted on Henrietta Lacks, a Black woman whose cells were reproduced without her permission. At the same time, researchers are understandably cautious.
“Because of Tuskegee, Henrietta Lacks and all of the bad things that have happened, we are still sort of concerned we might oversell the potential benefits of being in a research study, and we focus on the risks and potential downsides,” Randall said. “We are often overly focused on the downside and not enough on the upside.”
Challenges in accessing clinical trials
Sharon Rivera-Sanchez, a Triple Negative Breast Cancer (TNBC) survivor, participated in a clinical trial for breast cancer and shared her experiences on the panel. As the founder and director of the non-profit Trials of Color, she sees how raising awareness about colon and breast cancer among underserved and minority populations can change health outcomes. The organization is currently working with Massey Cancer Center and other groups to increase diversity in clinical trials, as part of Massey’s Community Grant Initiative.
Rivera-Sanchez says researchers need to acknowledge the apprehension among people of color, but also make sure they hear the potential positives of participating in these studies.
“We have to tackle what happened with Henrietta Lacks and Tuskegee,” Rivera-Sanchez said. “You [think of] the word ‘Guinea pig’ when a doctor or patient advocate brings up [clinical trials]. You have to be able to address that in a way that people can relate or understand it.”
According to a JAMA Network study, published by the American Medical Association, only about 5% of clinical trial participants were Black patients between 2015 and 2019. Study participants who identified as Hispanic were incorporated into other demographics.
Rivera-Sanchez says researchers should be finding ways to include everyone in a clinical trial and not find ways to exclude people. For example, some clinical trials have exclusions for participants with certain medical diagnoses and chronic illnesses, like diabetes which has predominantly been diagnosed in Black and Brown patients.
“Clinical trials are extremely important to find a cure. If it’s a medication trial, [we need to] find out if we have new medications that will work better,” Rivera-Sanchez said. “We always want to include our Black and Brown communities when we look at diversity [in clinical trials]. Plus our bodies are all different, so we don’t know if one drug will work on our [white] counterparts and will it really work on us.”
There are a number of barriers panelists noted that make it more difficult for people to be able to get involved in clinical trials. One of those is language. A large part of the United States population is Spanish-speaking, and Rivera-Sanchez says multiple language options are not always available in clinical trials.
Another barrier for some is transportation, with study participants often needing to travel to a trial site. This issue is starting to change. For clinical trials of COVID-19 medications, government officials allowed study participants to remain at home, and many are pushing the same opportunity for cancer research. Right now, Randall says, any patients who participate in her clinical trial must travel to Richmond.
“There are plenty of doctors out there in the state who are perfectly capable of giving a lot of these medications,” Randall said. “A patient could go locally. That would
tremendously increase enrollment. It would reduce the disparities of patients who can’t get to the center.”
Massey is working to make clinical trials accessible to more populations, particularly Black and Brown patients. Some of the center’s researchers are recognized as national leaders for their efforts to diversify clinical trials, receiving acknowledgements for innovative and inclusionary methods.
Approaching research opportunities with empathy and understanding
A cancer diagnosis is life-changing. Randall says researchers must be empathetic and listen to their patients to determine whether a clinical trial is a viable option. When Randall broaches the topic, she approaches the conversation as a doctor first, and the person running a clinical trial second.
“Every single person who comes through my doors, no matter what color or sexual orientation or what background they have, they all come from a very different place,” Randall said. “I try to listen to them more than I talk to them, and I introduce the idea of a clinical trial.”
One of the keys to increasing diversity in clinical trials is getting out of the research facilities and talking to people. Rivera-Sanchez says Massey and other cancer research organizations need more “boots on the ground” to talk to people and explain why participating in the study can benefit them.
The goal is for study participants to better mirror the diversity of the population, and that will create better data. This includes different age ranges, genders and races.
Randall says the federal government is starting to do a better job of pushing researchers to increase the diversity of study participants, but she notes that more needs to be done globally on these efforts. She believes Massey is really pushing forward with diversifying studies, and one of the reasons that’s happening is partnerships with organizations and community members, like Rivera-Sanchez and Trials of Color.