How to stop rising opioid overdose rates in the community during the COVID-19 pandemic
Miss America 2020 and a VCU Health researcher discussed opioid overdose numbers during the pandemic and offered advice on what you can do about it.
October 01, 2020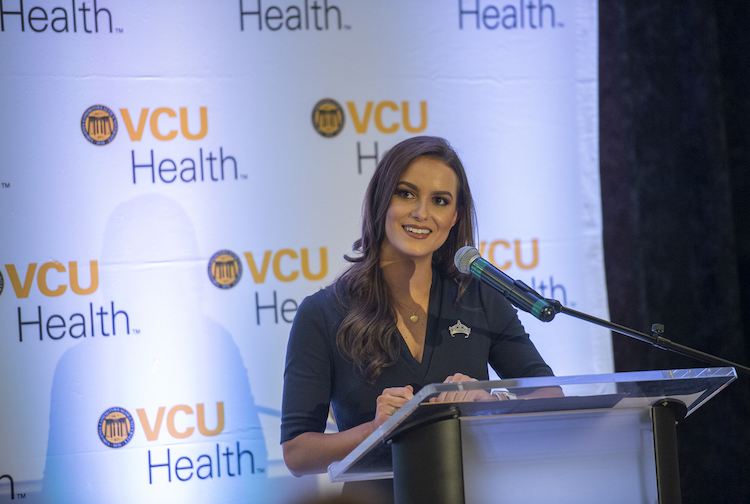
The COVID-19 pandemic has given way to a “very alarming number” of accidental opioid overdoses this spring, according to a VCU Health researcher. But, if you or someone you know is battling opioid addiction, you may not know where to turn, or perhaps the same resources you turned to in years past might not be available in the way that you’re used to.
Camille Schrier, Miss America 2020, and Taylor Ochalek, Ph.D., a VCU Health researcher, spoke virtually Tuesday about how to protect your loved ones, your community or yourself from rising opioid overdose rates during the pandemic.
“It’s sad that [the opioid crisis] is something that continues in our country and clearly is something that is worsening during the pandemic,” Schrier said. “And I think that it’s so important that we bring this to light.”
Schrier, also a graduate student in VCU School of Pharmacy’s Pharm.D. program, has spent her time as Miss America educating millions about medication safety and preventing the misuse of opioids through her Mind Your Meds social impact initiative. She spoke about Mind Your Meds to members of the VCU community in January, but on Tuesday, she — accompanied by Ochalek — turned her attention to a virtual audience across the United States on Instagram Live.
“August 31 was International Overdose Awareness Day, and September has been Recovery Month,” Schrier said. “I’ve spent a lot of time with those who either had a family member or are personally affected with substance use disorder, and we’ve been talking about how this is getting worse during the pandemic.”
Accidental overdose rates have climbed during the pandemic
Nonfatal accidental overdoses in March-June 2020 were up 123% over March-June 2019 at VCU Medical Center in Richmond, according to a recent study by Ochalek, a postdoctoral research fellow at the C. Kenneth and Dianne Wright Center for Clinical and Translational Research at VCU.
“[This] is a very, very alarming number, and I mean, it’s just shocking. And these are just non-fatal overdoses,” said Ochalek, who conducts research in the Department of Pharmacology and Toxicology and Department of Psychiatry at VCU Health. “This is data just from one hospital here at VCU, but this is definitely one example of something that’s probably a larger national trend in the U.S.”
The percentage of Black patients who came to the Emergency Department at VCU Medical Center while experiencing a nonfatal accidental opioid overdose also increased, from 63% last year to 80% this year during the same time periods, Ochalek said.
“Across the U.S., COVID-19 has really disproportionately impacted underserved minority populations, in terms of rates of the COVID-19 pandemic hospitalizations and deaths,” Ochalek said. “And with this data, from our sample, we found that opioid overdoses have actually also disproportionately impacted black patients. … And that’s a pretty alarming trend in a population that’s already experiencing really sad and alarming disproportionate rates of COVID-19-associated issues.”
What can you do about it?
One thing you can do, Schrier said, is to get trained to administer naloxone, also known as Narcan, an opioid overdose reversal medication that often comes in a nasal spray.
“In most states — I know in Virginia and here in Pennsylvania, where I am — you can get it through a state order. You might have to pay for it, or you can get it for free at a lot of distribution sites,” said Schrier, also a certified naloxone trainer in Richmond. “You can be the one to help turn that potential fatal overdose into a nonfatal overdose, and we can help people regain their lives.”
Virtual naloxone training is available, Ochalek said. If you’ve been waiting for the right time to get trained, various Virginia Department of Health districts locally have started offering online training on how to administer naloxone and how to recognize the signs of an overdose.
Safe disposal of unused medications at your local pharmacy or another drug take-back location can also help if you have a loved one who may be susceptible to opioid use disorder, Schrier said. The next National Prescription Drug Take Back Day is happening at locations nationwide later this month on Oct. 24.
While rehabilitation and hospitalized treatment are also options for those battling opioid addiction, Ochalek mentioned medication-assisted treatment with medications like buprenorphine or methadone as a possibility. These medications — intended to reduce opioid cravings and withdrawal symptoms — are often available at treatment centers, like VCU Health’s MOTIVATE Clinic, where patients work with doctors, social workers and other health professionals to return to their normal lives.
“With buprenorphine or methadone, there are treatment centers, and those significantly reduce the likelihood that someone’s going to overdose again,” Ochalek said.
But keeping the lines of communication open is one of the most important things you can do for a loved one who’s struggling with addiction, Schrier said, because there is “so much stigma association with addiction in general and substance abuse disorder.”
Ochalek echoed this advice from Schrier, noting that opioid use disorder often comes with withdrawal symptoms that can make a person feel sick. Some people continue to take opioids just to “maintain normalcy,” she said.
“One example that I often hear is you wouldn’t take insulin away from someone who has diabetes, right? You would give them their insulin. It’s a chronic disease,” Ochalek said. “So just like diabetes, opioid use disorder is a chronic disease. It’s a disease of the brain. And, fortunately, it is being more recognized. … It’s not just something that people can stop doing in a snap.”
Schrier said an important lesson she’s learned as Miss America, and formerly as Miss Virginia, is that some people who have stopped using opioids had a difficult time quitting because they realized they couldn’t pull themselves out of their addiction alone. Sometimes it was someone saving them from an overdose that helped them start to get better.
“I think one of the biggest things I’ve learned through this process is that not everyone’s recovery looks the same,” Schrier said. “But the biggest thing that you can do is to start.”
Resources for you or your loved ones
- Richmond Health District offers online naloxone trainings twice a week.
- Richmond Health District also offers free naloxone distribution by calling (804) 592-8069.
- Clear out your medicine cabinet; the next National Prescription Drug Take Back Day is Oct. 24.
- A number of local Drug Take Back locations accept unused prescription year round. Search by zip code to find a place nearby.
- If you’re not able to get to a Drug Take Back location but want to make old medications unusable, DEATakeBack.com has tips for how to dispose of these drugs at home.
- If you have a loved one who might live far away and needs in-person care, The Recovery Village, one of the Miss America organization’s national partners, has rehabilitation centers and recovery options across the U.S.
- The U.S. Department of Health and Human services offers virtual recovery resources at hhs.gov/opioids and its national helpline, (800) 662-4357.
- To contact VCU Health’s MOTIVATE Clinic about medication-assisted treatment for opioid addiction, call (804) 628-6776.
Additional local recovery programs
- The McShin Foundation, which helps those recovering from addiction and alcohol use disorder, is available at (804) 249-1845.
- The Healing Place, a part of Caritas, provides addiction recovery resources for homeless men. Call (804) 230-1184 for information.
- FCCR Rehabilitation Center has multiple specialized treatment locations in the Richmond area. Call (844) 696-4372.
- Substance Abuse and Addiction Recovery Alliance (SAARA) of Virginia offers services related to drug and alcohol addiction. Call (804) 762-4445.
- Hanover County Community Services Board has a 24-hour drug and alcohol crisis line at (804) 365-4200.
- Chesterfield Mental Health Services’ 24-hour mental health and substance use crisis line is (804) 748-6356.
- Henrico Mental Health and Developmental Services has a mental health and substance use crisis line available 24 hours a day at (804) 727-8484.
- Richmond Behavioral Health Authority’s 24-hour crisis line is (804) 819-4100.