Wright Center targets inequities in colorectal cancer screenings
Screening rates low in underserved communities.
November 29, 2021 Photo: Getty Images
Photo: Getty Images
Contributed by C. Kenneth and Dianne Wright Center for Clinical and Translational Research
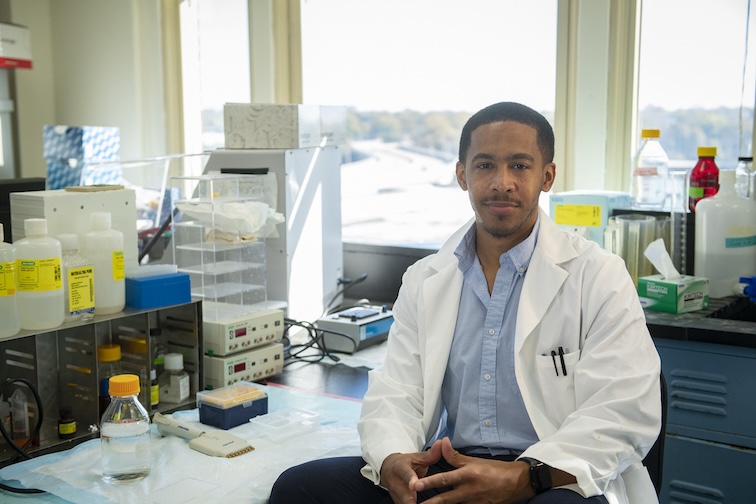
Growing up in rural southeast Arkansas, Michael Preston, Ph.D., M.P.H., saw the value of early screening for colorectal cancer firsthand.
His grandfather was screened early, and doctors were able to stop the cancer before it progressed. Preston credits the screening for his getting to enjoy many more years with his grandfather than he would have otherwise.

“I saw that as something that I wanted to address, and opportunity came along,” Preston said.
That opportunity was in Virginia, a state with 22 colorectal cancer hotspot counties of its own, where Preston took a faculty role at VCU in 2019. Now he’ll have the protected research time and funds to support his research through a new program, as the inaugural Wright Faculty Scholar in Health Disparities at the Wright Center for Clinical and Translational Research. The two-year award will support his work on programs that address colorectal cancer screening rates in communities where rates are low.
Community navigators — steering patients around health care hurdles
One program Preston is studying seeks to increase screenings through the use of community navigators who partner with patients to identify barriers. Navigators follow up with patients who’ve been recommended for screening but haven’t done so. They ensure patients are aware of their screening options (at home or at the clinic). And they work through barriers, like transportation to a doctor’s office or instructions for the take-home stool test.
“Navigators try to focus on the needs of the patient, their potential fears and knowledge of navigating the health care system, which can be very complex for most,” Preston said. “With men, there can be a ‘masculinity issue’ when it comes to colon cancer screening. Making them more comfortable about why it’s important to do this is the goal of the navigator.”
But are the programs working?
Preston’s primary research focus will be evaluating the effectiveness of those programs, especially in rural communities where health care often comes through federally qualified health care centers. These community-based clinics provide primary care services in underserved areas.
“Community health centers actually care for a lot of individuals in Virginia who are uninsured or under-insured,” Preston said. “A large number of individuals who haven’t been screened are in areas that are hard to reach, and the federally qualified health care centers are a great tool.”
Screening rates at Virginia’s 30 federally qualified health care sites vary from 14% to 63%. Preston hopes his research helps uncover the reasons for this variation. He’s keen to translate what he learns over the next few years into policy.
“Part of this project will be documenting and disseminating our findings to policymakers in a way that influences colorectal cancer mortality in Virginia,” he said. “Colorectal cancer is one cancer that you can actually prevent if people get screened. If we increase screening, we lower the number of people who die from colorectal cancer.”
“The pandemic only served to exacerbate previously unacceptable low rates of cancer screening in underserved areas. Dr. Preston’s research will be instrumental in helping raise those rates in Virginia for colorectal cancer with an ultimate goal of improving outcomes,” said Patrick Nana-Sinkam, M.D., Wright Center associate director and lead for the new scholar program. “The Wright Center is pleased to partner with him as our first scholar in health disparities and looks forward to supporting his research career.”